Not all Myocardial Infarcts (MIs) are the same – implications for Claims and Underwriting.
[In this article, the terms MI and Heart Attack are used interchangeably, as are high sensitivity Troponin (hs Tn) and Cardiac Troponin (cTn)]
Myocardial infarction refers to the death of myocytes (cardiac muscle cells), by deprivation of their blood supply. This will usually (but not always) be accompanied by symptoms such as chest pain and may result in cardiac arrest due to fast heart rhythms, such as ventricular tachycardia and ventricular fibrillation. Characteristic acute changes in the 12-lead electrocardiogram (ECG) occur, most commonly elevation of the ST segment.
As a result of myocyte death or injury, cardiac proteins leak into the bloodstream resulting in a characteristic rise and fall in the level of Troponin (I or T are the two types assayed). In the past, cardiac enzymes such as creatinine kinase were measured but Troponin (Tn) is more specific and has superseded enzymes as the biomarker of choice. An acute event will result in a dynamic change in Tn level (rise and/or fall), with the rise in Tn occurring within 3-4 hours after injury, peaking at around 18-24 hours, and remaining elevated for up to 2 weeks.
Refinements in laboratory technical ability have greatly improved the sensitivity of Tn assays such that smaller levels of Tn can be detected, so called high sensitivity Tn (hs Tn). The introduction of hs Tn has brought significant advantages for clinicians, effectively lowering the diagnostic threshold for MI, and allowing detection at an earlier stage. Since the implementation of hs Tn in clinical practice, it is estimated that there has been a 20% relative increase and 4% absolute increase in patients diagnosed with acute MI.
A rise in Tn, above the 99th percentile for healthy individuals, would be consistent with a diagnosis of MI in the right clinical context.
Arriving at the correct clinical diagnosis of MI requires careful evaluation of symptoms, ECG changes, laboratory data (Tn levels), imaging procedures, and sometimes pathological findings. It is important not to interpret Tn levels in isolation as they can be elevated in a wide range of conditions, both cardiac and non-cardiac.
Cardiac causes of elevated Tn include –
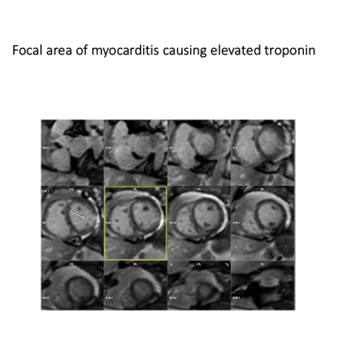
• Myocarditis – causes chest pain and ECG changes, which can mimic those of MI. Cardiac magnetic resonance (cMR) imaging can help differentiate between MI (abnormality seen in vessel territory - image 1) and myocarditis (injury seen outside of specific vessel territory - image 2).
• Cardiomyopathy – associated with chronic elevation of Tn.
• Heart failure.
• Heart block, Tachy – or Bradyarrhythmias.
• Cardiac contusion or other trauma, including cardiac surgery, pacing, ablation, and cardioversion.

Non-cardiac causes of elevated Tn include –
• Pulmonary embolism.
• Critically ill patients, especially sepsis, respiratory failure, and diabetes mellitus.
• Neurological injury such as stroke or subarachnoid haemorrhage cause catecholamine release and can also produce ST segment elevation on ECG.
• Renal failure.
• Skeletal muscle injury and strenuous exercise can elevate Tn levels, as skeletal muscle also contains Tn.
Classification of types of MI
(cTn denotes cardiac Troponin)
Type 1 - Classic myocardial infarction
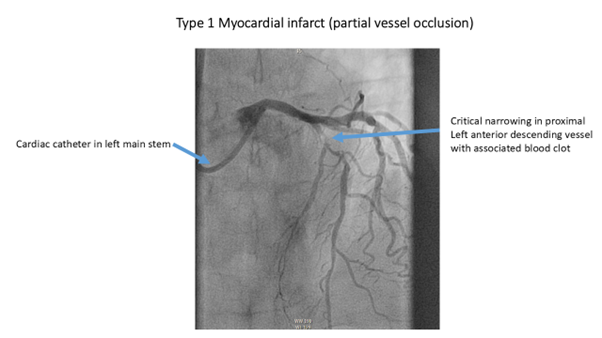
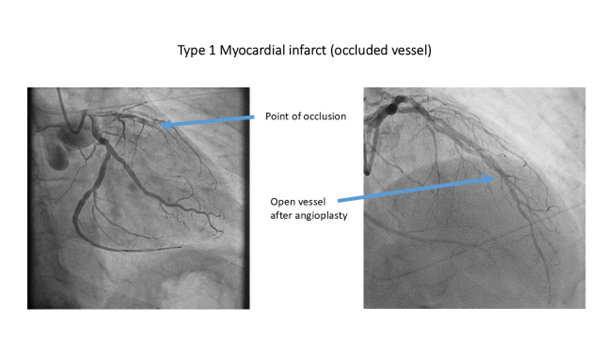
Occlusion of a coronary artery resulting in myocardial infarction (OMI), and non-occlusive myocardial infarction (NOMI) due to plaque rupture without vessel occlusion, are referred to as Type 1 myocardial infarction. If there is sufficient damage, echocardiography will show regional wall motion abnormalities (RWMA), and cMR can visualise the area of damage.
The criteria for Type 1 MI, according to the Expert Consensus Document on the Fourth Universal Definition of Myocardial Infarction (MI), includes detection of a rise and/or fall of cTn with at least one value above the 99th percentile and with at least one of the following:
• Symptoms of acute myocardial ischaemia.
• New ischaemic ECG changes.
• Development of pathological Q waves on the ECG.
• Imaging evidence of new loss of viable myocardium or new RWMA in a pattern consistent with an ischaemic aetiology.
Identification of a coronary thrombus by angiography including intracoronary imaging.
Type 2 - Myocardial injury due to imbalance between oxygen supply and demand
Clinical conditions which reduce the myocardial perfusion (e.g. severe hypotension or shock) or those which increase the myocardial oxygen demand (e.g. sustained tachycardia such as AF, or severe hypertension) can cause myocardial injury resulting in a rise in the cTn. In this situation, the clinical presentation is key to making the correct diagnosis and applying the correct treatment. As a result of implementation of hs Tn, the number of patients diagnosed with type 2 MIs has doubled.
The criteria for Type 2 MI includes detection of a rise and/or fall of cTn with at least one value above the 99th percentile and evidence of an imbalance between myocardial oxygen supply and demand, unrelated to coronary thrombosis and with at least one of the following:
• Symptoms of acute myocardial ischaemia.
• New ischemic ECG changes.
• Development of pathological Q waves.
• Imaging evidence of new loss of viable myocardium, or new RWMA in a pattern consistent with an ischemic aetiology.
It is increasingly recognised that some patients experience MI with normal or near normal coronary arteries on angiography (≤ 50% stenosis in a major coronary artery). Myocardial infarction with non-obstructive coronary arteries (MINOCA) disproportionately affects women and may account for up to 50% of MIs in women < 55 years of age. MINOCA is more commonly seen in non-Caucasian individuals, and those affected are less likely to have the typical cardiovascular risk factors such as hypertension, diabetes, smoking and hyperlipidaemia. There are several recognised causes of MINOCA including coronary artery spasm, which can occur spontaneously or following the use of illicit drugs e.g. cocaine.
This article focuses on the two main types of MI (Type 1 and Type 2) seen by Underwriters and Claims Assessors. However, there are other types of MI, particularly Type 4a and 4b, which are briefly covered below. Type 3 MI refer to MIs diagnosed at death, and Type 5 MIs are associated with coronary artery bypass grafting. Details of these can be found at Assessment and classification of patients with myocardial injury and infarction in clinical practice | Heart
Type 3 – Myocardial Infarction - diagnosed at death
Type 4 a – Myocardial Infarction with percutaneous coronary intervention (PCI)
Type 4 a - PCI may cause a rise in cTn, and this form of cardiac procedural myocardial injury is arbitrarily defined by increases of cTn values (> 99th percentile Upper Reference Limit/URL) in patients with normal baseline values (≤ 99th percentile URL) or a rise of cTn values > 20% of the baseline value when it is above the 99th percentile, but it is stable or falling.
Type 4 b – Myocardial Infarction with stent thrombosis associated with PCI
Type 4 a & Type 4 b are both iatrogenic related MIs, and in addition to the cTn rise, they require one of the following:
• New ischaemic ECG changes.
• Imaging evidence of new loss of viable myocardium, or RWMA in a pattern consistent with an ischemic aetiology.
• Angiographic findings consistent with flow limiting complications, such as coronary dissection or vessel thrombus.
Type 5 – Coronary artery bypass grafting (CABG) - related Myocardial Infarction
Comparing Type 1 and Type 2 MIs
Studies comparing Type 1 with Type 2 MI patients, reveal statistically different patient characteristics and outcomes, including:
• Type 2 MI patients are older than Type 1 MI patients.
• Type 2 MI patients have a higher prevalence of comorbidities, such as heart failure, AF, and kidney disease.
• Rates of intervention, such as PCI and CABG are lower among Type 2 MI patients.
• Type 2 MI patients have a significantly increased risk of all–cause death compared to Type 1 MI patients, in both the short-term and long-term. This increased risk is likely reflective of more comorbidities in the older Type 2 MI patients.
What is the relevance of these different types of MIs for Insurers?
Heart Attacks are a very common cause for claims on Critical Illness (CI) policies. The policy definitions for Heart Attack have evolved over time with successive generations of policies. These changes were developed by the ABI, CI working party, and were reflected in the Statements of Best Practice, and latterly, the Guide to Minimum Standards.
The older definition requires evidence of heart muscle death due to inadequate blood supply, as evidenced by chest pain, new ECG changes, and a rise in cardiac enzymes/Tn. Subsequent policy definitions included a “severity threshold” for Tn, reflecting the introduction of hs Tn by clinicians, and with it the diagnosis of more MIs, many of which would formerly have been diagnosed as “unstable angina”.
Insurers frequently see claims for MI where cTn measurements are below the policy threshold. In these cases, the advice of a CMO may be required to determine if the trajectory of cTn readings would have exceeded the threshold, if measurements had been obtained at the peak time.
Claims for patients who have presented to hospital with MIs associated with ST segment elevation on ECG (STEMI) will usually not have had cTn levels measured. This is because the diagnosis of STEMI requires only symptoms suggestive of MI and confirmatory ECG evidence (ST segment elevation). The priority in these cases is for rapid reperfusion of the myocardium by primary PCI (image 4), and cTn evidence is not required.
In recent years, many Insurers have adopted a stripped back policy definition for Heart Attack without the severity threshold for cTn. Although this type of definition is commendably brief, it is very loose.
Originally, when critical illness policies were priced, they were based on the classic Type 1 MI. However, the classification of MIs has expanded with different types being described, and the introduction of hs Tn has led to a doubling in the number of Type 2 MIs being diagnosed. Given the changing pattern of MIs, one might expect an impact on the pricing of CI plans. However, many insurers do not collect data, to differentiate between the different types of MIs at the claims stage. The extent of any impact can only be established with detailed biometric data of the numbers of MI claims broken down into the various types.
Current underwriting guidelines do not differentiate between Type 1 and Type 2 MIs, which have significantly different patient characteristics and outcomes. Type 2 MI patients tend to have a higher prevalence of comorbidities, with differing prognostic implications. The underwriting of applications for Life Cover in these individuals, may require expert guidance.
Author: Dr Paul Foley, Consultant Cardiologist & Dr Peter O’Connell, Emergency Medicine Consultant (Retired),
Company Medical Advisers Ltd.
Contact: Admin@companymedicaladvisers.co.uk
Last updated: 16/12/2024
References: available on request.
Company Number 7789011. Company Registered in England & Wales.
Registered Office: 186 High Street, Winslow, Buckinghamshire MK18 3DQ
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.

